Breastfeeding Depression Ncbi
International breastfeeding journal 2 6. Its considered safe for breastfeeding.
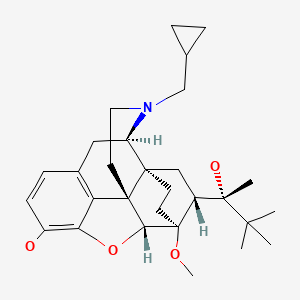
Buprenorphine Drugs And Lactation Database Lactmed Ncbi Bookshelf
Maternal or Infant Illnesses or Conditions.
Breastfeeding depression ncbi. Vaccinations Medications Drugs. Breastmilk is the ideal form of nutrition for infants. It is comparatively safe antidepressants while breastfeeding which has a short half-life but which might lead to withdrawal symptoms such as dizziness gastrointestinal disturbances insomnia headache dry mouth constipation sedation antimuscarinic side effects or.
In that studys conclusion the authors state that women who present depressive symptoms before or after childbirth are at high risk to discontinue breastfeeding. Chamomile tea is a caffeine-free beverage made with boiled water and dried flowers of the chamomile herb. However the research examining the association between postpartum depression and breastfeeding has been somewhat difficult to interpret.
However the direction and precise nature of this relationship are not yet clear. However more research is needed to confirm these findings. The adult vulnerability to depression may have its origins in early childhood.
This can be achieved through social support from family and healthcare providers. To assess these relationships the current study aims to examine the association between prepregnancy depression and breastfeeding duration by maternal age. A new paradigm for depression in new mothers.
The purpose of this paper is to provide an overview of the relationship between breastfeeding and postpartum depression as it has been examined in the empirical literature. Emerging research suggests that a relationship exists between breastfeeding and postpartum depression. Pregnancy depression predicts a shorter breastfeeding duration but not breastfeeding intention or initiation.
Research on the association between pregnancy depression and breastfeeding initiation remains equivocal with one study showing no association between the variables Bogen et al 2010 and two studies suggesting that depressive symptomatology during pregnancy and pregnancy depression predicted shorter breastfeeding initiation Figueiredo et al 2014. There is a need to manage antenatal postnatal depression in mothers in order to encourage them to initiate breastfeeding earlier and to breastfeed for longer. As the level of depression of women increases in the postpartum period the level of breastfeeding self-efficacy decreases.
Traumatic births can make breastfeeding more difficult and can cause a delay to the milk coming in due to high levels of stress hormone cortisol Kendall-Tackett. If you are a patient we strongly advise that you consult with your physician to interpret the information provided as it may not apply to you. The tea is known for its soothing taste and therapeutic properties.
Further it has also been suggested that breastfeeding may offer protective benefits against postpartum depression 28. In breastfeeding women the risk-benefit balance of pharmacological therapy is altered and antidepressant therapy should only typically be considered if the woman has expressed a preference for medication declines psychological interventions if her symptoms have not responded to psychological interventions or if she has a history of severe depression. Conclusion Depression is negatively associated with breastfeeding practices.
Another important aspect addressed in that meta-analysis was the association between short breastfeeding duration depression during pregnancy and PPD. Postpartum depression can be prevented when parents are given positive parenting lessons and when the maternal-infant bond is promoted and increased. It also may help improve an infants cognitive development.
According to a 2018 systematic review by the Agency for Healthcare Research and Quality AHRQ external icon Elucidating the relationship between breastfeeding and postpartum depression is challenging because women with depression may have difficulty initiating and sustaining breastfeeding and women who experience breastfeeding difficulties may develop. Studies show breastfeeding or chestfeeding reduces risk of sudden infant death syndrome SIDS by 50 at all ages throughout infancy. One large study of over 2500 women.
Its nutritional composition uniquely caters for the health and growth needs of a baby 13. Higher rates of postpartum depression. Traumatic birth can be associated with depression or post traumatic stress disorder PTSD particularly if the mother is already prone to depressionCounselling for a traumatic birth can be very helpful.
The central role of inflammation and how breastfeeding and anti-inflammatory treatments protect maternal mental health. Studies have claimed that exclusive breastfeeding during infancy reduces the risk of depression in adulthood. The breastfeeding self-efficacy increases as the level of social support increases and as the attitudes that drive breastfeeding behavior change positively.
Mothers with a high risk of depression were less likely to have a positive attitude towards breastfeeding OR 037 95 CI 0199 0675 as compared to mothers with a low risk of depression p 001. References Breastfeeding and reduced risk of sudden infant death syndrome. Thus examining the influence of prepregnancy depression on breastfeeding may help providers identify and appropriately intervene with women in age groups at highest risk of premature cessation.
Breastfeeding mothers consider chamomile tea for its anti-depression anti-anxiety anti-inflammatory and galactagogue effects. Understand the potential problems of sudden breastfeeding cessation and know how to properly advise mothers on the management of breastfeeding while taking medicines. Although postpartum depression has been identified as a risk factor for early breastfeeding cessation early negative breastfeeding experiences may be a risk factor for postpartum depression.
We found that there is an association between the risk of depression and the attitude towards breastfeeding. Postnatal depression was associated with shorter duration of exclusive full and any breastfeeding P 001. There is recent evidence that suggests women with difficulty breastfeeding may be at risk for postpartum depression.
Many question if breastfeeding may protect against postpartum depression and if the cessation of breastfeeding is a trigger for postpartum depression andor anxiety. It can re-regulate the thyroid adrenal glands a common concern postpartum Its effective in helping if you have anxiety fatigue cloudy thinking and insomnia. But most of these effects are inadequately.
Infants who are never breastfed are at a higher risk of depression and hostility in adulthood. Other studies suggest that breastfeeding may reduce the risk for certain allergic diseases asthma obesity and type 2 diabetes. Exclusive breastfeeding has a positive effect on reducing depressive symptoms from childbirth to 3 months.
Breastfeeding duration is associated with postpartum depression in almost all studies. Lactation Category C or compatible with breastfeeding by Mills Bones ³. Postpartum depression predicts and is predicted by breastfeeding cessation in several studies.
Postpartum Benefits of using Ashwagandha.
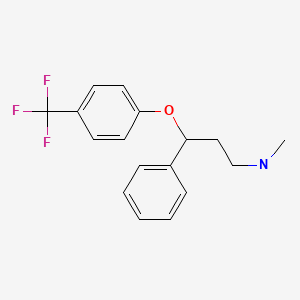
Fluoxetine Drugs And Lactation Database Lactmed Ncbi Bookshelf
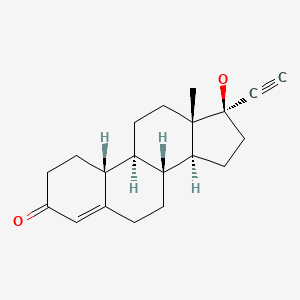
Norethindrone Drugs And Lactation Database Lactmed Ncbi Bookshelf
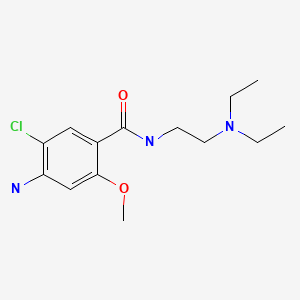
Metoclopramide Drugs And Lactation Database Lactmed Ncbi Bookshelf
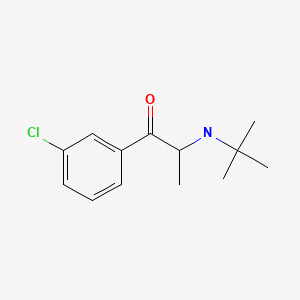
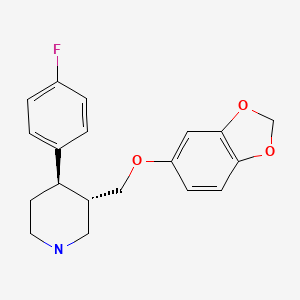
Paroxetine Drugs And Lactation Database Lactmed Ncbi Bookshelf
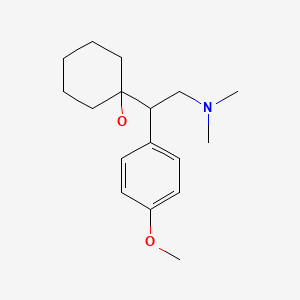
Venlafaxine Drugs And Lactation Database Lactmed Ncbi Bookshelf
Posting Komentar untuk "Breastfeeding Depression Ncbi"